Nutrition in early life is known to be a key determinant of immediate neonatal survival and for subsequent growth and mental development during infancy; it is also a major conditioning factor for long-term health1-3. Preterm infants have greater nutritional requirements than their term-born peers, the extent of which varies according to the degree of prematurity and weight at birth. Meeting these specific requirements calls for tailored nutrition specific to each case.
TAILORED NUTRITION, KEY TO PRETERM INFANTS’ LONG-TERM HEALTH
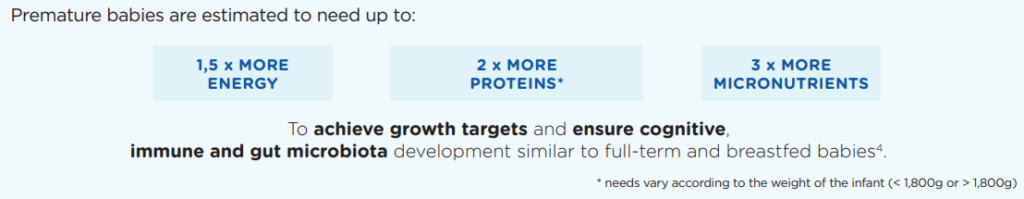
Just at the time when their absorptive and digestive capacities are limited, preterm infants have greater nutritional needs. These needs vary according to the degree of their prematurity, their weight and their stage of development 4-7.

Without adequate nutritional support, prematurity can give rise not only to complications at birth but also to long-term cognitive and psychomotor difficulties.
Prolonged delays in growth or excessively rapid weight gain have also been associated with greater risks of metabolic disease5,8.
Preterm infants therefore require a diet which is adapted to their needs and adjusted continually according to their developmental progression.
PERSONALISED NUTRITIONAL SUPPORT IN LINE WITH ESPGHAN* RECOMMENDATIONS
Taking into account their greater and changing nutritional needs, ESPGHAN* has established specific recommendations for the diet of preterm infants, according to their weight and stage of development and their access to breast milk (see diagram).
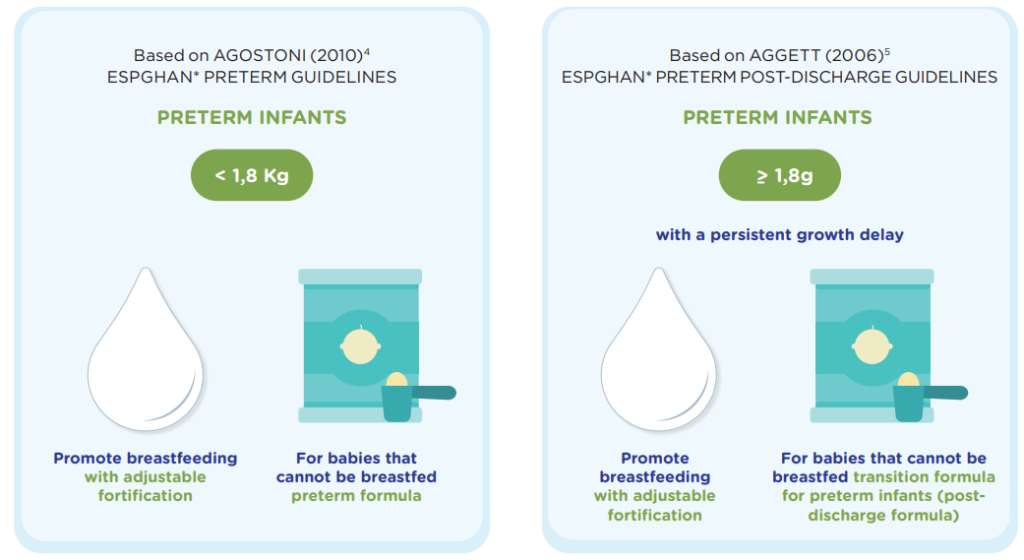
It should be noted that the extent of breast milk fortification and the duration of specific post-discharge transitional feeding should be decided upon on the basis of close monitoring of the infant’s growth. Once growth goals have been met and appropriate growth has been achieved, the transition to unfortified breast milk or standard infant formula should be suggested.
“Every effort, including use of preterm formula, is justified to protect the preterm infant from growth failure and the neurodevelopmental impairment it engenders” (E.E. Ziegler 201510)
APTAMIL PRE NUTRIPREM and APTAMIL NUTRIPREM PDF: TAILORED FORMULAS FOR PRETERM NON-BREASTFED INFANTS
Drawing on 70 years of accumulated expertise in prematurity and 50 years of research on breast milk, Nutricia offers, for the first time in Africa, a tailor-made nutritional solution, designed according to ESPGHAN recommendations*4,5 to meet the specific needs of non-breastfed premature infants.
Hence Aptamil Pre Nutriprem formula for premature infants <1,800g and Aptamil Nutriprem PDF formula for preterm infants over 1,800g who are experiencing a persistent delay in growth:
- Offer a flexible solution that enables nutritional intake to be adapted according to the infant’s weight and stage of development;
- Meet the increased protein and energy needs of preterm infants;
- Are enriched with a patented mixture of scGOS:lcFOS*** (9:1), clinically demonstrated to mimic the oligosaccharides found in breast milk, and with nucleotides, which together support the development of the gut microbiota and the immune system11-15;
- Contain readily absorbable medium-chain triglycerides16;
- Provide, in sufficient quality and quantity the LC-PUFAs** necessary for brain development17-19 in a form easily absorbed and incorporated into the tissues20,21.
References
*ESPGHAN: European Society for Paediatric Gastroenterology Hepatology and Nutrition
** Long Chain Polyunsaturated Fatty Acids
*** scGOS / lcFOS: short chain galacto-oligosaccharides / long chain fructo-oligosaccharides
- Gruszfeld and Socha. World Rev Nutr Diet. 2013;108:32-9.
- Demmelmair et al. Early Hum Dev. 2006;82:567-74.
- Wrottesley et al. J Dev Orig Health Dis. 2016;7:144-62.
- Agostoni et al. J Pediatr Gastroenterol Nutr. 2010;50:85-91.
- Aggett et al. J Pediatr Gastroenterol Nutr. 2006;42:596-603.
- American academy of pediatrics. 2014. In Kleinman, RE & Greer, FR (Eds.), Pediatric nutrition (7th ed., Vol. Section II: Feeding the infant, pp. 83-110). Elk Grove Village, IL, USA.
- Ziegler EE. Ann Nutr Metab. 2011;58 Suppl 1:8-18.
- Kerkhof et al. Clin. Endocrinol. Metab.2012;97:4498-4506
- Lapillonne et al. ArchPediatr. 2011 ;18: 313-323.
- Ziegler EE. J Pediatr Gastroenterol Nutr. 2015;61 Suppl 1:S3.
- Boehm G et al. Arch Dis Child Fetal Neonatal Ed 2002; 86:F178-81.
- Knol et al. Acta Pædiatrica, 2005; 94(Suppl 449):31–33.
- Westerbeek et al. Am J Clin Nutr 2010;91:679–86.
- Bruzzezes et al. Am J Clin Nutr 2010;91:679–86
- Singapore Med J. 1998;39:145-150.
- Marten et al. Int Dairy J. 2006;16:1374‐82.
- Koletzko et al. Karger Medical and Scientific Publishers, 2014. 110:201–214.
- Schuchard and Hahn. Woodhead Publishing, 2011. 32-78.
- Willatts et al. Am J Clin Nutr. 2013;98: 536S-542S.
- Carnielli et al. Am J Clin Nutr. 1998;67:97-103.
- Liu et al. JLipid Res. 2014;55:531-9.
BA21-681
