Parental reassurance and education, along with advice on nutritional management in infants, are the first steps in treating infant regurgitation.
NASPGHAN* and ESPGHAN** provided an update of their clinical guidelines for the diagnosis and management of gastroesophageal reflux (GER) and gastroesophageal reflux disease (GERD) in infants and children. These guidelines address both pediatric gastroenterologists and primary care physicians.
The first-line management of infant regurgitation should start with parental education and reassurance, as recommended by NASPGHAN/ESPGHAN and other pediatric experts on functional gastrointestinal disorders (FGIDs). Placing infants in a prone, anti-Trendelenburg sleeping position (with the head higher than the feet by 10°) is not recommended because of the risk of sudden infant death syndrome (SIDS).
Recommendations on parental education and reassurance:
- Expert group review1: provide parents with information on the natural history of regurgitation (even in breastfed infants), correct formula preparation (in formula-fed infants) and overfeeding intensifying symptoms
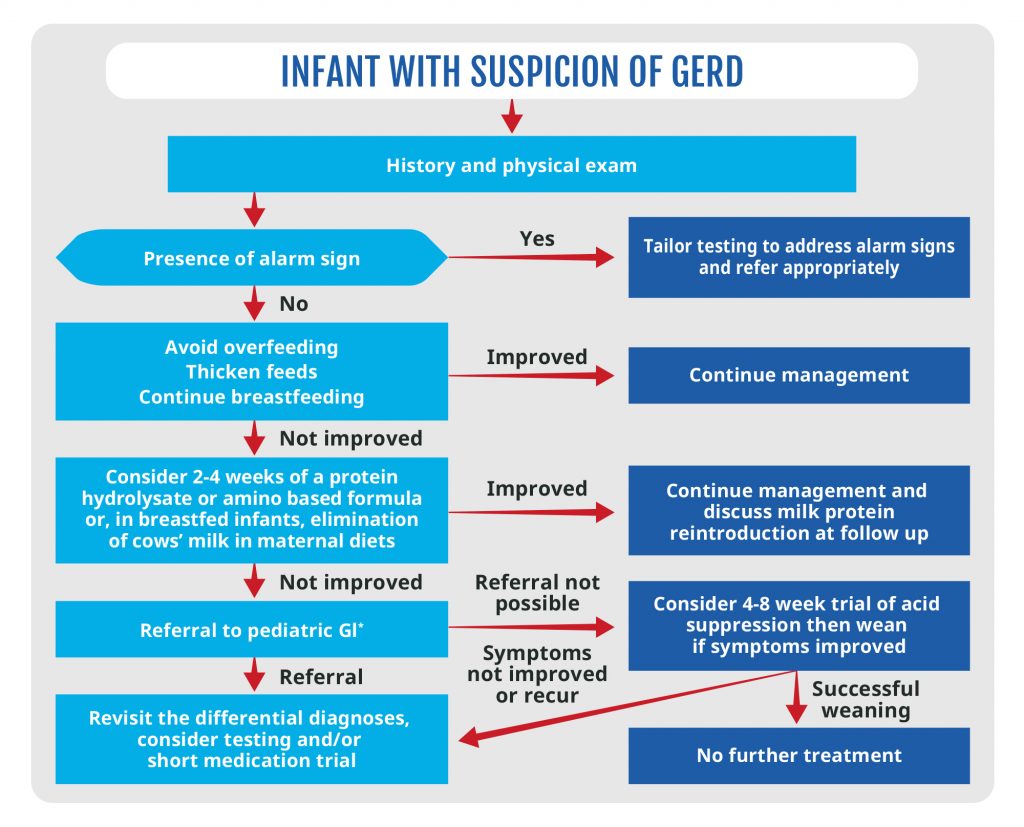
- NASPGHAN/ESPGHAN2: in most infants, supine positioning during sleep is recommended. The second step should look at nutritional management. NAPSGHAN/ESPGHAN developed an algorithm for the management of recurrent regurgitation (figure 1).
*GastroIntestinal
Pharmacological therapy for infant regurgitation
Some facts on pharmacological therapy in cases of infant regurgitation:
- Most cases resolve spontaneously, with complete resolution in 95% of infants by one year of age3
- The efficacy is debatable: proton pump inhibitors have no effect on crying and irritability in infants4, pharmacological treatment of infants with reflux symptoms is problematic5
- Adverse effects: include headaches, diarrhea, nausea and constipation6; long term use of PPI (Proton-Pum Inhibitor) may directly or indirectly affect the gut microbiome7; significant association between PPI use and risk of dysbiosis/SIBO (small intestinal bacterial overgrowth8)
Current recommendations
These are excerpts of current recommendations on pharmacological therapy by different expert organizations:
- NASPGHAN/ESPGHAN2: no pharmacological treatment of crying/distress or visible regurgitation in otherwise healthy infants; proton pump inhibitors (PPI) only in cases of gastro-esophageal reflux disease (GERD), prescribe the lowest doses for the shortest possible length of time
- Expert group review1: no indication of drug treatment in ‘happy spitters’ or in infants without troublesome regurgitation; PPI do not decrease infant regurgitation, crying or fussiness and should not be empirically started
- NICE9: no acid-suppressing drug (e.g. PPI or Histamine-2 receptor antagonists) to treat overt regurgitation in infants and children occurring as an isolated symptom
- No pharmacological therapy for infant regurgitation in otherwise healthy children, only moderate use in case of a clear diagnosis of GERD
*North American Society for Pediatric Gastroenterology, Hepatology and Nutrition
**European Society for Paediatric Gastroenterology, Hepatology and Nutrition
References
- Vandenplas, Yvan, et al. “Functional gastro‐intestinal disorder algorithms focus on early recognition, parental reassurance and nutritional strategies.” Acta Paediatrica 105.3 (2016): 244-252.
- Rosen, Rachel, et al. “Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition and the European Society for Pediatric
- Hegar, Badriul, et al. “Natural evolution of regurgitation in healthy infants.” Acta pædiatrica 98.7 (2009): 1189-1193.
- Gieruszczak-Białek, Dorota, et al. “No effect of proton pump inhibitors on crying and irritability in infants: systematic review of randomized controlled trials.” The Journal of pediatrics 166.3 (2015): 767-770.
- Olarte Parra, Camila, et al. “Cochrane database of systematic reviews.” (1996).
- Goulooze, Sebastiaan C., Adam F. Cohen, and Robert Rissmann. “Should be there specific guidelines to improve reporting of clinical pharmacology trials?.” Br J Clin Pharmacol 80.2 (2015): 175-175.
- Vesper, B. J., et al. “The effect of proton pump inhibitors on the human microbiota.” Current drug metabolism 10.1 (2009): 84-89.
- Su, Tingting, et al. “Meta-analysis: proton pump inhibitors moderately increase the risk of small intestinal bacterial overgrowth.” Journal of gastroenterology 53.1 (2018): 27-36.
- National Institute for Health and Care Excellence, London: NICE, 2015
BA19-485